Health Hub
Symptoms, diagnosis and treatments for wrist pain conditions (including carpal tunnel syndrome)
Checked for accuracy by Mr Rupert Wharton

Wrist pain can arise from various conditions, each requiring specific treatments for effective relief.
Since the onset of the COVID-19 pandemic, there has been a notable increase in carpal tunnel syndrome (CTS) cases, making it a major cause of wrist discomfort. However, CTS is just one of many conditions contributing to wrist pain.
This article aims to guide you in understanding and finding the right treatment for a range of wrist pain issues. To help in this endeavour, we spoke to Mr Rupert Wharton, a consultant Trauma and Orthopaedic surgeon here at King Edward VII’s Hospital. He specialises in sports injuries and degenerative conditions of the hand and wrist.
Mr Wharton helps us to understand the symptoms, diagnostic processes and treatment options for various conditions to help you get the best health outcome.
Jump to the following sections:
- Carpal tunnel syndrome
- Basal thumb arthritis
- De Quervain’s tenosynovitis
- Other conditions that can cause wrist pain
- Other ways to treat and manage wrist pain.
Get in touch if you want to find out more about treatments for your wrist pain.
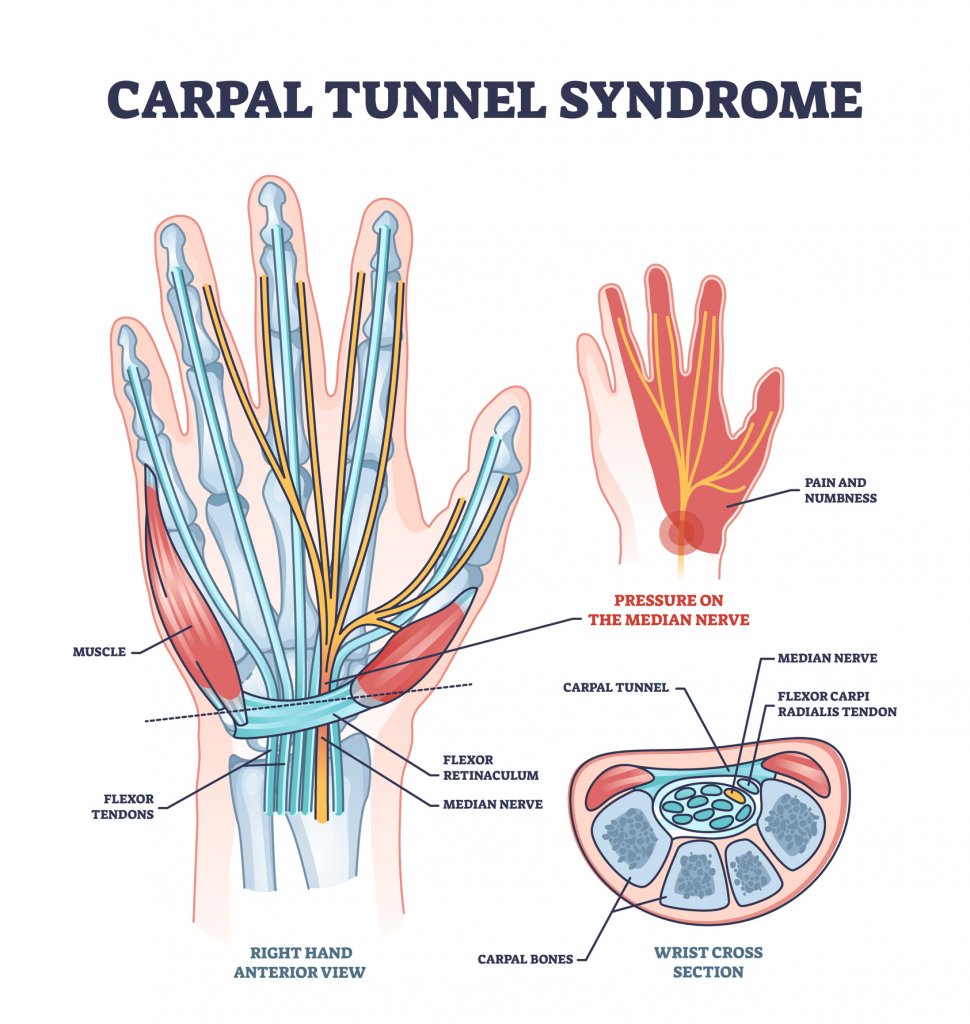
Carpal Tunnel Syndrome
Carpal tunnel does not always give people wrist pain. It can cause pain in the front of the forearm sometimes. More commonly, people get a tingling in the fingers of what’s usually described as the ‘radial three’: the three fingers on the thumb side of the hand.
People frequently say that their fingers go numb. They wake up at night and they have to shake their hand to get rid of the pain or tingling – or it becomes painful in a particular position. This loss of sleep can be really disturbing for people.
It can be difficult for patients to identify exactly which fingers are affected when they wake up in the middle of the night. Often they only complain of a tingling of the fingers, but as the condition progresses, they can often identify that it’s in the radial three. When we point out that the ring finger has been relatively spared on the other side, it’s a pretty conclusive diagnosis of CTS.
As it progresses though, the median nerve, which runs through the carpal tunnel, affects the thenar muscles in the hand. These muscles are crucial because they allow you to move your thumb forward. If these muscles weaken, you won’t be able to move your thumb properly, making it difficult for the thumb to work together with the other fingers.
Thumb function is about 50% of your hand function in general. If you can’t power your thumb properly away from the fingers, that’s a real problem; you won’t be able to pinch your thumb and fore-finger so fine motor tasks will become difficult.
People find that the tingling really affects them when they’re trying to do dexterous tasks. It becomes very difficult to button up a shirt. Writing becomes difficult because the sensation is unpleasant – it feels like pins and needles.
Carpal tunnel syndrome diagnosis
Our job in the clinic is to understand how long symptoms have been going on and to try and grade it – classify the severity of the symptoms.
Part of grading is to understand whether the symptoms come and go or whether they’re continuous. We also need to understand how much the thumb musculature is affected.
This is so we can understand the best treatment as there are a number of options.
Carpal tunnel syndrome treatment options
If symptoms come and go and the thumb muscle is okay and if the power of the thumb muscle is okay, then we consider some non-operative treatment in the first instance because the patient will have time as the condition hasn’t progressed that far. If symptoms persist, you may wish to consider Carpal Tunnel Release Surgery
Splinting
In this case we would usually recommend a non-operative option – sleeping with the wrist in a splint.
Commonly people buy a splint off the shelf. These splints are usually designed for people who have injured their wrist so they tilt back 30 degrees because that’s a functional position for the wrist and the wrist likes to be in that position.
However, if you have carpal tunnel syndrome, the wrist should be straight because that’s the position at which the pressures in the carpal tunnel are at their lowest. We recommend that people who have purchased off-the-shelf splints bend it into position. They are usually aluminium so it’s easy to do.
Splints mean patients can sleep with their wrist in a splint that will reduce the pressures in the carpal tunnel. This is important because many people bend their wrists when they sleep and this puts pressure on the median nerve in the carpal tunnel, which is not good if it’s already irritable.
Physiotherapy
Physiotherapy can play a limited role. Sometimes simple exercises to keep the nerve moving – bending the wrist forward and back, and moving the fingers up and down – can be effective. This is to ensure that the tendons don’t get stuck onto the nerve. This can happen due to inflammatory change in both the tendons and the nerve, and if they all get stuck together it can cause a lot of pain when they start to move.
Find out more about physiotherapy at King Edward VII’s Hospital.

Steroid injections
The next step is to discuss steroid injections which can help both diagnostically and therapeutically.
Steroid injections are helpful diagnostically, because, if somebody responds really well to a steroid injection – even if it’s transient – that tells us a) that the problem is coming from the carpal tunnel, and b) that they’ll usually respond equally well to an operation.
Relief is temporary. It might last six weeks, three months or in rare cases it might last a year or even solve the problem. However, if symptoms return, we can be pretty confident that the problem is in the carpal tunnel, that we will need to operate and that that will solve the problem.
So, while relief can be temporary, it guides diagnosis and informs what we might do next.
Surgery: carpal tunnel decompression.
If symptoms are permanent and don’t improve, this is a concern, because it suggests that the nerve is constantly under pressure, that it’s not getting a good blood supply. This can mean a race against time to alleviate the pressure on the nerve – especially if the patient starts to get wasting of thumb muscles. This means we need to operate as soon as possible.
The operation – carpal tunnel decompression – is our most common operation in hand surgery. It’s done under local anaesthetic and takes us about 10 minutes. Patients come in and go home on the same day.
We inject the palm near the wrist with local anaesthetic. When it takes effect, patients can move it but feel no pain. We make a small incision and move the muscle out of the way. We divide the thick compressive ligament that’s causing the problem by squashing the nerve. This removes the problem. When this is done we sew the skin back up again.
Patients usually have a bulky bandage or dressing around their hand for five days, which they can take off themselves at home. A small dressing is usually fine for the following two weeks. After this they can go back to using their hand as normal.
The success rates from carpal tunnel decompression are well in advance of 95% as long as we’ve got the right diagnosis.
During recovery, the fingers will try to stiffen up so it’s really important that patients do finger movement exercises afterwards. This is so that the nerve doesn’t get stuck down onto the tendons as everything’s inflammatory after the surgery.
Find out more about carpal tunnel release surgery
Covid and the rise of carpal tunnel syndrome
There’s been an explosion in both the prevalence of carpal tunnel syndrome (CTS), but also in its severity. NHS waiting lists for carpal tunnel syndrome treatment are long and only getting longer.
This may be related to the virus – we saw a lot of COVID-related neuropathy. For example, some people would get a wrist-drop following a bout of covid which would get better by itself.
That would be a problem usually related to the posterior interosseous nerve – which is a branch of the radial nerve. For some reason, being affected by the virus, you get an inflammatory change in the nerve and the nerve goes on strike. This means the muscles that lift the wrist up seem to fail temporarily. The nerve then recovers over a few weeks and they get better.
If that happens to the radial nerve, it could also happen to the median nerve running through the carpal tunnel – the nerve that’s affected in carpal tunnel syndrome.
As such, we’ve seen a dramatic increase in the number of people with CTS seeking treatment.
Carpal tunnel decompression surgery makes up half of the wrist operations people are waiting to have done.
Basal thumb arthritis (also base-of-thumb arthritis)
The second most common condition that results in wrist pain is basal thumb arthritis which affects the carpometacarpal joint directly underneath the thumb. This involves the thumb metacarpal. Downstream of it, there’s the carpometacarpal joint, and just underneath that is another joint called the scaphotrapeziotrapezoid (STT) joint. The condition particularly affects women after the menopause.

The problem is usually related to ‘pinch’ over many years. When you pinch, studies suggest that you put 12 times your body weight through that carpometacarpal joint. That’s a huge amount of force over a small surface area. So, if you have basal arthritis, you’ll develop pain down the thumb ray – along the length of the thumb. Patients usually find that when they pinch, it’s very sore. Activities like opening jars, turning door knobs and using a knife and fork to cut meat become painful.
Basal thumb arthritis treatment
We use a splint called a PUSH or a Jura prosthesis, which is very effective.
If that doesn’t work, then the hand therapy exercises can be helpful – certainly for the long-term control of your pain. We ask patients to put a rubber band around their fingers and then push outwards against their fingers. This strengthens the first dorsal interosseous muscle, which is a stabilising muscle for that joint.
When the splint isn’t helping anymore, we discuss steroid injections.
If steroids fail and symptoms that remain painful are affecting quality of life, we discuss surgical options.
There are three main operations that we would do for basal arthritis:
- Trapeziectomy – In this operation, we cut out the trapezium bone (the small bone at the base of the thumb). Outcomes are fantastic after six months, often following some niggling pain.
- Thumb CMC replacement – This joint replacement surgery involves removing the damaged bone and cartilage in the CMC joint and replacing it with an artificial implant. The goal of the procedure is to reduce pain, improve joint function and restore thumb mobility.
- CMC fusions – This procedure involves permanently fusing the bones in the affected joint to alleviate pain and provide stability. We recommend this for younger patients who need to get mobile due to physical work.
There’s no one-size-fits-all procedure when it comes to hand surgery options. This is why it’s essential to meet people. We spend a long time getting to know patients, understanding what drives them, what their functional status is like, what their expectations are from treatment and what they want to achieve. Once we know this, we can tailor our treatments.
READ: 39 Things You Can Do To Help Prevent Arthritis
De Quervain’s tenosynovitis
De Quervain’s is an inflammatory condition of the tendon that runs down the thumb.
We see this condition, particularly in people who move their thumb a lot for work. It is often an overuse condition in people who do a lot of typing for work.
Treatment
The treatment options include:
- Splinting
- Steroid injections
- Physical therapy
- Surgery (surgical release similar to carpal tunnel decompression)
Other conditions that can cause wrist pain
- Ganglion cysts
- Wrist fractures
- Tendonitis
- TFCC (triangular fibrocartilage complex) tears
- Rheumatoid arthritis
- Osteoarthritis
- Wrist sprains
- Kienbock’s disease
- Gout
- Psoriatic arthritis
- Repetitive strain injury (RSI)
- Carpal boss
- Intersection syndrome
- Wrist drop
- Tenosynovitis.
Other ways to treat and manage wrist pain
- Rest to avoid activities that exacerbate the pain.
- Ice and heat therapy – Apply ice packs for acute pain or heat packs for chronic pain to reduce inflammation and alleviate discomfort.
- Medication
- NSAIDs (non-steroidal anti-inflammatory drugs): Ibuprofen, naproxen.
- Analgesics: Acetaminophen.
- Topical pain relievers: Creams or gels containing capsaicin or menthol.
- Injections – Hyaluronic acid injections for osteoarthritis.
- Activity Modification:
- Ergonomic adjustments to workstations.
- Modifying techniques in sports or daily activities to reduce strain.
- Acupuncture
- Chiropractic care – Manual adjustment to improve joint function and reduce pain.
- Massage therapy to relax muscles and improve circulation.
- Occupational therapy to teach proper hand and wrist movements and reduce strain during daily activities.
Get in touch to discuss any musculoskeletal conditions you may have and we can help you find the best treatment.
Article Sections
Latest Hospital News
Should you wish to speak to our press team, please visit Press Enquiries





