Steve’s story
Steve Robinson was in constant pain. He had good days and bad days. But the Centre for Veterans Health Pain Management Programme has helped Steve both understand and manage his pain so that he can have more good days than bad.

Brother in arms
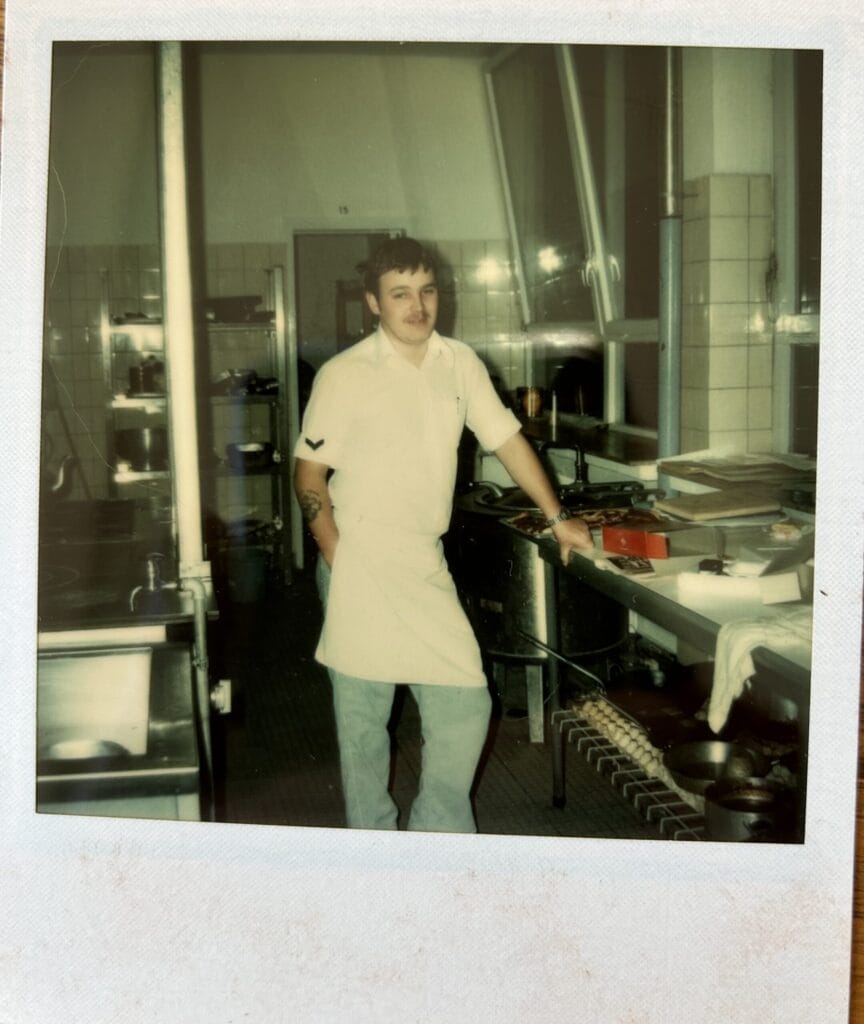
Steve Robinson is from South Manchester but has been around the world with the military. Today he lives in Lancashire with his wife and two children. Steve’s Army career started in 1991 with the Royal Corps of Signals. He took his training and excelled – noticed by his superiors as a promising recruit.
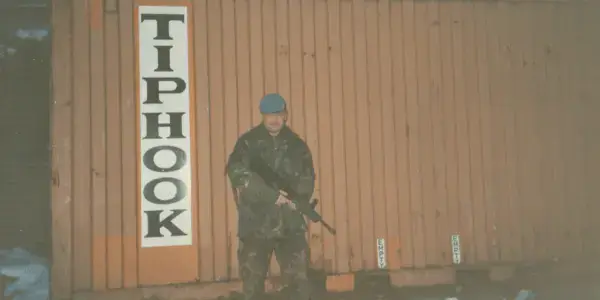
By 1993, he had been deployed to central Bosnia as war raged. When he wasn’t in a warzone he was training in places from the Alps to the Arctic.
It was during this training that Steve sustained a bad injury, dislocating his arm in a skiing accident. “It took them three and a half hours to get me off the mountain,” he says. “They managed to get my shoulder back in, but I was out of action, so they sent me back to the UK.”
Back at the Woolwich Hospital in London, they reconstructed Steve’s shoulder using experimental new surgery, which went well. Even so, Steve was recovering for eight months, including three weeks at the Army’s rehabilitation centre, Headley Court.
Getting his back up
“Once I’d recovered, they asked me: where do you want to go? We’ll send you anywhere you want,” explains Steve. “I wasn’t sure as I was spending lots of time getting fit again. Within a month I was back in Bosnia – deployed in autumn 1995.”
It was at this time that Steve’s back started to degrade and developed sciatica in his right leg (pain, weakness, numbness, or tingling in the leg. Caused by injury to or pressure on the sciatic nerve). “We didn’t have a field hospital so I was just given ibuprofen.
“My back got worse. I was in agony,” he says. “It got so bad that I couldn’t move. I was driven cross country for several hours to reach a hospital in Gornji Vakuv and they diagnosed me with two prolapsed discs. My boss saw me and said, “right, you’re going home.” Ominously, Steve alludes to another condition that was creeping up on him – a subtle and hidden condition.

Steve was treated at the Royal Hospital Haslar, Hampshire. He was discharged but still in pain and told to head home. “I was ‘sick, lame and lazy’,” he says in the parlance.
Steve describes one of the problems with medicine in the military: “If you have a leg blown off, it’s easy to see. If you have something invisible, like back pain, they can be dubious about it. There can be a suspicion that you’re faking it for whatever reason.” This was pertinent to Steve’s agonising physical pain, but even more relevant to another condition that while invisible was no less powerful – still hidden from Steve’s own view.
In 1996 Steve was sent for surgery in Coventry where he received a double discectomy. The operation was a success and reduced his pain, though his movement was still restricted. Steve’s lifelong drive to get active and get outdoors helped him rehabilitate and while he couldn’t run, he was able to tackle the Matterhorn on one of two Alpine trips.
“Things were ok and I was enjoying life again,” he says. “However, I knew that, in my present condition, I wouldn’t ever get promoted to sergeant because I wouldn’t be able to complete the one-year course. I knew I’d stay where I was and that my Army career would be over fairly soon.”
“I’d been with the 30 Signal Regiment for four and a half years – their longest-serving member. I couldn’t stay any longer. They had to post me out, so I went to RAF Balado Bridge in Scotland.”
Unfortunately for a man of action like Steve, while he was close to his beloved mountains, the work culture was one of inactivity.
For better or worse, fate would intervene. “In 1998, I was called in to see a surgeon. He said ‘you can’t do your job. Do you want medical discharge? I said ‘yes’. By the time I’d got back to base, my superior had been informed and I was out of the Army.”
Civvy street
Steve and his wife moved back to England where his character and experience saw him soon excelling as Operations Manager at then telecommunications giant Marconi PLC. While Steve’s drive and ambition now had an outlet, and one that bore fantastic fruit, he was still frequently suffering from sciatica and pain.
In 2002 Steve’s life changed again when he and his wife upped-sticks and bought a gastro-pub. While it was yet another business success, Steve’s back started to get much worse. It had happened on and off for some years, but his mental health was suffering again and Steve was prescribed antidepressants but refused to take them.
Steve’s experience of the local NHS was poor and, in desperation, he explored his private options. Back surgery would cost £7,000 but the consultant said they could fix the issue so he went ahead.
While the surgery had its complications, his back settled and notwithstanding little flare ups, Steve got his life back. While he couldn’t run or lift weights, he could stay active – essential for a man with such passion for the outdoors and the kind of vigorous activity the military offered, from mountaineering to skiing.
Hidden trauma
But that nameless, obscure condition was getting worse – hidden but always present. “I put on weight. I had no energy. All that drive I’d always had seemed to be slipping away from me.
“Then I had a heart attack,” he says, light as a feather. After a dramatic blue-light journey and medical response, the issue solved – at least, his heart attack was.
“I’d be walking down the street and some loud bang would send me back to Bosnia – I was getting flashbacks. It wasn’t talked about back when I was in the Army, but I realised I probably had PTSD. Experiencing the devastation of war, seeing children suffer and being constantly under threat.”

Formal diagnosis came in 2016 and gave Steve clarity as well as a pathway forward. In total, he spent 13 weeks being treated by Combat Stress at Hollybush House in Scotland where he received “superb treatment”.
His cardiac rehab started with speed walking and long walks but before he knew it he was up Ben Nevis and even discovered a passion for cave diving – scuba diving plus potholing. He quit the rat race and worked for Belisama’s Retreat, an organisation that helps veterans with PTSD, getting them out into nature: camping, tracking, building fires, “real caveman stuff”.
The theatre
In 2021 Steve’s back got worse again. The consultant said that it wasn’t bad enough to operate on, but that if Steve should suffer any numbness, loss of control or incontinence, he should go straight to A&E. The consultant gave him a card saying: ‘present this when you get to A&E and they’ll get you straight through…’.
“In May of 2022 I had been in for an MRI scan. Ten days later I woke up, headed for the toilet, but I didn’t make it. I told my wife that we needed to go to A&E and we started packing a bag. Then the phone goes. It’s the neurologist, he says, ‘Come in straight away. We need to get you into surgery, now!’.
“After five hours of waiting on the floor, they finally found me a bed.
Days of chaos ensued with surgery and delays and MRIs and more delays – confusion and uncertainty.
“I get back to my bed after being visited by a friend. I’m packing, ready to leave. A doctor comes in, all panicking. ‘I think we need another MRI’. I’m thinking this is going to mean another day waiting in hospital but within thirty minutes she’s back in and says, ‘we need to operate, now!’. Within three minutes the whole surgical team was there and took me back into theatre. Turns out I had a massive blood clot. The doctor that saw that in my MRI saved my life.”
Shortly after surgery, Steve is discharged. He can’t control his foot, can’t walk, he’s incontinent and gets constant agonising stabbing pains in his foot. The pain triggers his PTSD. Opioids only offer some relief.
Never give in
Steve was in pain, both chronic and acute. But, as he says, “I have a complete and utter refusal to give in.” Through a veterans Facebook group, Steve learned about the King Edward VII’s Hospital and our Centre for Veterans’ Health (CFVH). He researched our Veterans’ Pain Management Programme and his application was successful. The course includes daily virtual sessions with eight other veterans and specialists as well as private sessions as required. The programme lasts 10 full days – the first nine days being completed within seven weeks, the final day of the programme taking place nine months later.
“The best thing about the Pain Management Programme is the knowledge, the understanding that it’s given me,” explains Steve. “I feel like, if I can understand something, I can control it.
“Pain is the body’s way of saying that there’s something wrong. But sometimes the body gets it wrong, sends pain when there’s nothing wrong. So, when I get an attack, instead of worrying about what’s wrong, I know I just have to ignore the pain. The pain is a ghost – it’s not real.
“I’ve also learned about my triggers, because it’s not logical – it’s not just about overuse or knocks, getting a cold or flu can also trigger the pain.
“The medication review is also fantastic. The specialists will talk to you about what you’re taking, what’s working, what’s not, make recommendations. It’s all very tailored to the individual. They also helped me reduce my reliance on opiates – using them more tactically. You just don’t get that kind of expertise and attention anywhere else.”
Steve has also found immense value in meeting other vets with similar problems. While the mutual support and community is great, it’s also a valuable source of practical advice as people share their experience – sharing tips and coping strategies that have worked for them.
“The KEVII specialists challenge the orthodoxy, the one-size-fits-all approach to medicine. They tailored exercises and my regimen based on my situation – it’s all personalised.”
We ask Steve, how are you feeling today?
“Today is a good day. I’m in pain but it’s not too bad. It’s under control, I’m managing it and that’s because of the programme.”
That and his ‘complete and utter refusal to give in’.

Help support our charitable work with Armed Forces veterans.
Are you inspired by the stories you’ve read here and wish to make a donation to the Centre for Veterans’ Health?
100% of donation to the Centre for Veterans’ Health, go directly to support veterans.

Since 1899 King Edward VII’s Hospital has supported members of the Armed Forces. We continue to uphold this commitment today.
For information, contact Caroline Dunne - Coordinator of the Centre for Veterans’ Health, at cdunne@kingedwardvii.co.uk.
All Service or ex-Service Personnel (including reserves) without medical insurance are eligible for a 20% discount on hospital fees. This also applies to their spouses, civil partners, widows, and widowers.
More stories
If you require surgical treatment, our world-famous centre of excellence is able to treat the full spectrum of knee conditions and complaints.
You can be seen by a specialist quickly and at a time that suits you, with same day appointments often available.