Lucy’s story
Lucy Holt had lived in pain for years. What started on the netball court was followed by multiple surgeries and medical discharge. While her mysterious ankle injury was solved, the pain never ended.
Her ankle is still on the road to recovery, but the Veteran’s Pain Management Programme has helped her reclaim her life.

A sports injury
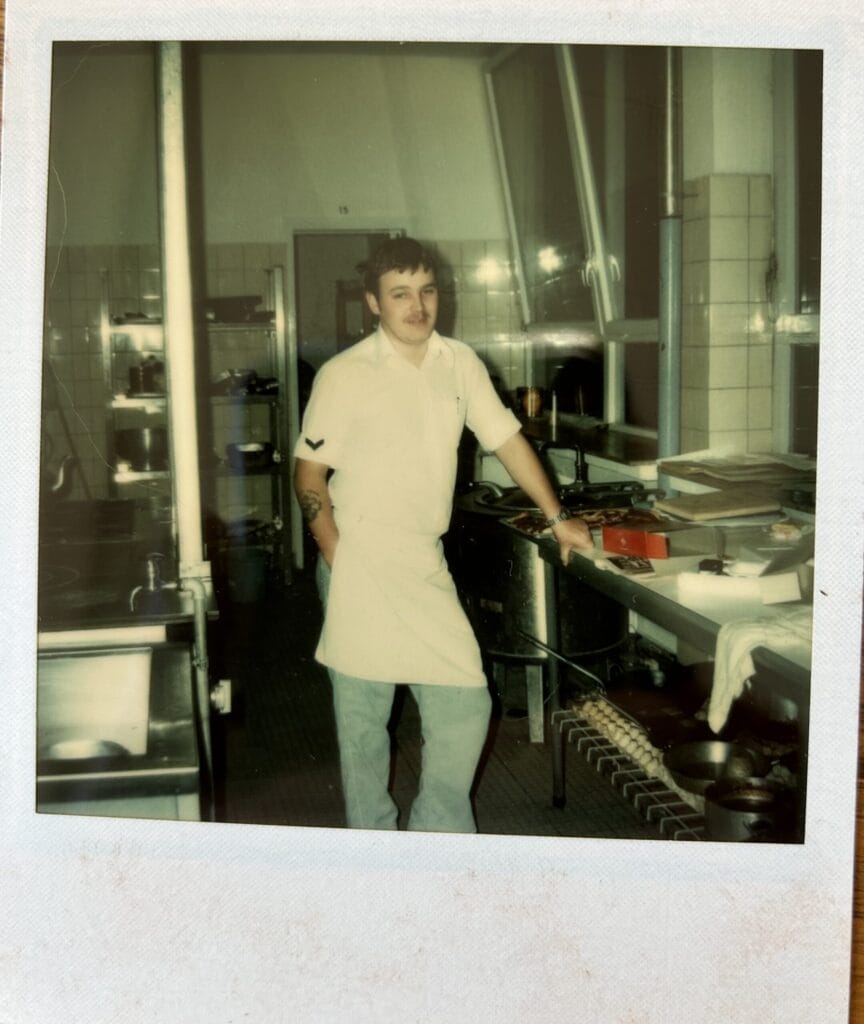
Lucy Holt joined the Royal Air Force (RAF) as a steward when she was 16, back in 2009. She was initially based at RAF Cottesmore in Rutland but has since been stationed at both Brize Norton in Oxfordshire and RAF Odiham in Hampshire.
“I really enjoyed my work,” explains Lucy. “I got to work with lots of different people from the officers’ mess and sergeants’ mess to VIP duties and the Station Commander’s house.”
In 2016 Lucy sustained an injury while playing netball. “I went over on my ankle. It hurt but I thought it was just a sprain. I took a break from netball and hoped that it would get better on its own.”
But it didn’t.
Back at work, Lucy was working a large function working from 7am until 2am.

“I wore my boots until 7pm. Then we changed into formal dress for the meal service. I was in my formal shoes and I kept rolling my ankle.
“The next morning I was up at 7am. I couldn’t put my shoes on. I couldn’t put any weight on my ankle. The medics said I might have broken my foot.”
Lucy was sent for scans and tests but the x-ray revealed that the foot wasn’t broken.
“I was up on crutches but no one knew what was wrong.”
The physiotherapist sent Lucy for an MRI which showed that nothing was broken and that it must be muscular – a bad sprain. Lucy was recommended rehabilitation and attended Headley Court – then an armed forces rehabilitation centre.
“My ankle was still giving way on a regular basis and no one could work out why, or why it wasn’t healing,” explains Lucy, who was sent for more scans.
The mystery persisted and Lucy returned to base and was put on sedentary duty – away from service, behind a desk – from March until May 2016.
“In 2018 I went back to Headley. I was told I was unfit for service and was medically discharged,” says Lucy, the emotion clear in her voice as she describes what happened. “You told me there’s nothing wrong with me because you don’t know what’s wrong with me. But you’re also saying I’m unfit. It didn’t make sense. It was a tough pill to swallow.
“I was sent home for a second time so I sat at home doing nothing for two years. I was P0 Non-Effective – a medical status that is given to personnel who are no longer able to do their jobs within the military and are sent on long-term sickness before going to a medical board.”
Lucy continued her medical journey throughout 2018 with a variety of appointments and checkups – all the time in chronic pain.
A mystery solved
In a final attempt to find out what was wrong, she was referred to a consultant in Basingstoke.
“He did loads of x-rays and scans in the morning,” says Lucy. “Then, in the afternoon he said: I don’t know what it is, but I know it’s bad. We need to operate… tomorrow’.”
They opened up Lucy’s ankle on either side. Only now was the damage clear.
“It turned out I had a 7.5cm tear in my peroneal tendon and that three out of four ligaments were completely ruptured. There wasn’t much holding onto my ankle.”
An operation that October seemed to be successful, but the access wound itself failed to heal, so Lucy was yet again in surgery. But the wound would not heal and she was left with a two centimetre deep hole in her ankle. And so Lucy was again referred, this time to a major trauma centre in London where she saw a major trauma surgeon.
This surgery revealed that the reason that the wound would not heal was that the blood supply to the ankle was damaged and not functioning properly. This was due to the long delay in having it properly diagnosed and treated.
“I was with the orthopaedic surgeon, then the plastic trauma team – back and forth between London and Lincolnshire.”
The team tried lots of different approaches, including a suction dressing to promote healthy tissue growth. “They worked until they took the dressings off.”
More surgery followed in 2019 including one lasting 10 hours that aimed to promote healing by moving the blood supply in her foot and utilising a skin graft from her leg. Lucy spent the following week in the major trauma centre and then again, back and forth weekly to have her wound checked and dressed. She also went to Cornwall for physiotherapy, which she says was great.
“I didn’t know if I would ever walk again,” says Lucy.
Since 2018, Lucy has had nine surgeries to her ankle. Her last surgery was in January 2023 and, at the time of writing (February 2024), she is due one final surgery.
Pain management
“In 2019, the big surgery severed many of the neural pathways which left me in a lot of pain. I had…” Lucy pauses as she describes the condition. “It’s hard to explain. I get different sensations in my foot. If you touch my skin graft, I feel it in my foot. It’s horrendous and the pain was constant.”
Even the smallest knock would leave Lucy in agony and genuinely concerned as to whether she had caused new damage to her ankle.
“My doctor was very patient with me. He’d put me through all the tests and reassure me that I hadn’t caused any more damage. But still the pain was insufferable. I needed something.
Lucy’s orthopaedic consultant knew the King Edward VII’s Hospital and told her about our Veterans’ Pain Management Programme. “He told me that the programme was funded by the Centre for Veterans Health and that I could apply apply for the free programme. He explained that applications were judged by a panel and that it wasn’t guaranteed, but I had a good case. I was desperate. I’d try anything that might be able to help – I was always in such pain.
“He sent a letter on my behalf, outlining everything I’d been through and that he thought I might have complex regional pain syndrome. He got the ball rolling. My GP emailed and I also sent them some information. Within a week I’d been accepted and had received the welcome pack and was reading through to understand what would happen on the course.
Taking back control
“Their aim was to help me manage pain in the moment.”
The initial stage of the course started every day at 9am and finished at 3pm and included a range of methods to tackle pain, including yoga and mindfulness sessions – all delivered virtually through video calls.
“It was great to be able to do the sessions from home,” says Lucy. “It was nice to be in a group with others like me, but really convenient at the same time.”

The course also included support for emergencies, medical appointments and medication reviews if requested, as well as sessions with any of a team of six specialists, for example, a psychologist and pain specialists.
The first week is every day, followed by a break and then 19 days spread over the following six months. This includes reactive sessions as required. “I could just get in touch with the administrator to book in a session if I wanted to talk to someone. The team was great. So friendly. They’d speak to me about my immediate situation and get me in touch with someone who could help.
“The course isn’t about fixing you,” says Lucy. “It arms you with a set of tools for coping with pain – managing it day to day.
“The course helps you set goals and build towards them. On day one you can’t get out of bed. And maybe you can’t on day two. But by day 20 you can. And it’s all because you have that toolkit.
One of Lucy’s goals was to walk around the golf course with her son. And did she reach that goal?
“I did!” she beams. “The course helped me remove the psychological walls that chronic pain puts up between you and things you want to do. The course helped me build resilience and take back control of my life.”
And take control she has, getting involved with the Invictus Games through which she hopes to gain teaching qualifications so she can work with disabled children.

We ask Lucy what she’d say to other veterans who may be dealing with chronic pain.
“If you’ve done a pain management course but it didn’t work, then apply for KEVII’s Veterans’ Pain Management Programme. Disregard what other courses have said or done and go into KEVII’s with an open mind because it’s completely different. They will welcome you with open arms and support you in every way they can. It was an amazing experience.”
Help support our charitable work with Armed Forces veterans.
Are you inspired by the stories you’ve read here and wish to make a donation to the Centre for Veterans’ Health?
100% of donation to the Centre for Veterans’ Health, go directly to support veterans.

Since 1899 King Edward VII’s Hospital has supported members of the Armed Forces. We continue to uphold this commitment today.
For information, contact Caroline Dunne - Coordinator of the Centre for Veterans’ Health, at cdunne@kingedwardvii.co.uk.
All Service or ex-Service Personnel (including reserves) without medical insurance are eligible for a 20% discount on hospital fees. This also applies to their spouses, civil partners, widows, and widowers.
More stories
If you require surgical treatment, our world-famous centre of excellence is able to treat the full spectrum of knee conditions and complaints.
You can be seen by a specialist quickly and at a time that suits you, with same day appointments often available.