Health Hub
What is macular degeneration and how is it best treated?
Checked for accuracy by Mr Saruban Pasu

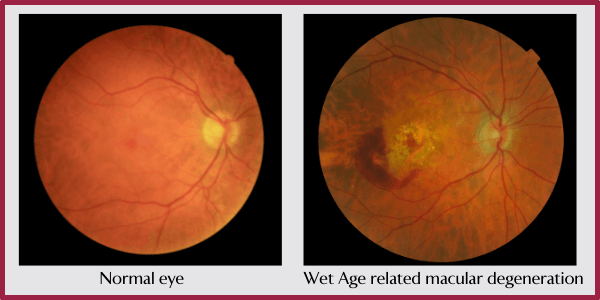
Macular degeneration, often also referred to as age related macular degeneration, is a long term disease of the macular. The macular is the small, central part of the retina at the back of the eye that’s responsible for the clear, central vision in your direct line of sight.
There are two different forms – wet macular degeneration and dry macular degeneration. The condition is most common in people over the age of 50 years old and the risk increases as you get older. Someone aged 50 to 59 years old has an increased risk of 2% of developing the condition whereas someone who is over the age of 75 has a 30% increased risk.
It’s the most common cause of visual impairment in older people and can cause significant upset and disruption to quality of life and independence. Here, we speak to King Edward VII’s Hospital Consultant Ophthalmologist, Mr Saruban Pasu, about the condition and how it’s best treated.
What are the different types of macular degeneration?
Dry macular degeneration is the most common form of the condition and can develop in one or both eyes. If it develops in one eye, there’s a greater risk it will also develop in the other eye.
It’s characterised by the development of small, yellow deposits called drusen, under the retina. Drusen are a normal consequence of the ageing process, but in macular degeneration, they begin to grow both in number and size.
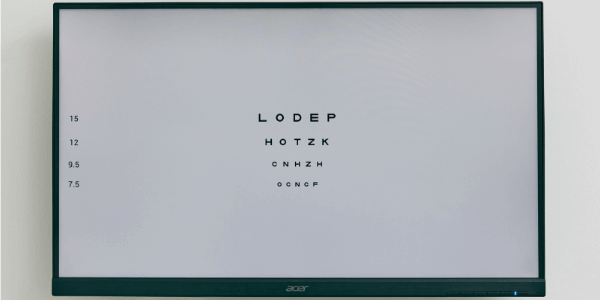
They can be detected during a normal eye examination with an optician or a specialist eye examination with an ophthalmologist. Over time, larger and more prolific drusen can cause damage to the macular, causing vision to deteriorate. This macular deterioration can then reduce your vision and affect your ability to do normal things such as reading, driving and recognising the finer details of people’s faces.
It doesn’t necessarily mean that you’ll lose all of your sight. But most commonly, people with dry macular degeneration notice that their central vision becomes impaired, whilst their peripheral vision remains the same. Vision loss with dry macular degeneration may be mild, whilst in others, it may be severe.
Dry macular degeneration can progress into wet (neovascular) macular degeneration. Wet macular degeneration is less common, and means that blood vessels have grown under the retina and have begun to leak blood.
The dry form of the condition usually slowly progresses over years, and causes a gradual decline in vision. However, wet macular degeneration can cause a relatively sudden change in vision resulting in serious central vision loss. (Like dry macular degeneration, wet macular degeneration doesn’t affect the peripheral vision.)
What causes macular degeneration?
The exact cause of macular degeneration is still unknown but there are some lifestyle factors that can increase your risk of developing the condition. These include:
- Smoking or being regularly exposed to cigarette smoke
- Being very overweight or obese
Age is a large factor in the condition – as we age, the tissue within the macular area can begin to thin, as cells responsible for vision are lost. Other factors that may increase your chance of developing macular degeneration include:
- Having a close family member with the condition
- Being Caucasian
What are the symptoms of macular degeneration?
Since macular degeneration only affects the central vision, as opposed to the peripheral vision, the first sign is usually blurring or distortion in the central part of your vision (the part directly in the centre of where you’re looking, as opposed to your side view). This can occur in one or both of your eyes and can present itself as:
- Wavy, blurred or distorted lines of text on a page or screen when reading
- Straight lines looking wavy or bent
- Blurry areas on a printed page or screen
You may also notice:
- Difficulty ready or seeing finer details in low light levels
- Difficulty watching TV, reading, driving or recognising people’s faces
- Extra sensitivity to glare
- General blurred vision
- Things looking smaller than they are
- Colours appearing less bright than they are
If your symptoms get worse, you may have complete dark spots in the centre of your vision where you can’t see anything. Macular degeneration doesn’t cause any pain or discomfort, or change the external appearance of your eyes.
How long does it take to lose vision with macular degeneration?
Dry macular degeneration can become advanced and cause loss of vision without becoming wet macular degeneration. However, it is also possible for early stage dry macular degeneration to suddenly become wet macular degeneration.
Dry macular degeneration can take years to significantly affect your vision, but wet macular degeneration can cause a sudden change in vision. Therefore, regular eye tests, particularly as you get older, are an important tool for monitoring your eye health.
The best way to manage dry macular degeneration is to speak to your optician or ophthalmologist about any changes to your eyes or your vision. One way to monitor your central vision at home is to use the Amsler Chart. It’s important that you inform your optician or ophthalmologist of any changes.
If your optician suspects that you may have macular degeneration, you will be referred to an eye specialist straight away, as the sooner treatment is started, the less risk you have of developing significant visual impairments.
How is macular degeneration diagnosed?
Macular degeneration can be spotted during a routine eye test, or via a specialist eye test with an ophthalmologist.
Optical coherence tomography (OCT) is a non-invasive imaging test that uses light waves to take pictures of the retina at the back of your eye. During this test, your optician or ophthalmologist will be able to see each of the distinctive layers of the retina and is considered the Gold Standard of diagnosing macular degeneration.
An OCT test is now a routine part of a regular eye test at an opticians, which is why regular eye tests are so important, even if you don’t wear glasses.
Are there certain foods that might help macular degeneration?
Eating a healthy diet rich in fruits, vegetables, wholegrains and lean proteins is good for overall health.
If you have macular degeneration then you may especially benefit from eating foods that are high in antioxidants called lutein and zeaxanthin. These foods include kale, spinach, broccoli and squash. You may also benefit from foods such as lean meat, shellfish, chickpeas, lentils, beans, nuts and seeds that are rich in zinc.
What treatments are available for macular degeneration?
Macular degeneration cannot be reversed. However, the progression of the dry form of the condition can be slowed down if caught early enough, by eating a healthy diet and quitting smoking if you smoke. There are various clinical trials that are currently in progress looking into treating dry macular degeneration.
There is, however, treatment available for wet macular degeneration. VEGF, or vascular endothelial growth factor, is a protein that helps new blood vessels to develop and grow. Anti-VEGF medications can be injected into the back of the eye, to help prevent the growth of new, weaker blood vessels in the eye that can leak blood and make macular degeneration worse by causing scar tissue.
Anti-VEGF injections may sound daunting, but they can help to stop the progression of wet macular degeneration and prevent significant vision loss. They stop the condition from getting worse in 9 out of 10 people and improves the vision of 3 out of 10 people with wet macular degeneration.
These injections are usually given every one or two months, and the eyes are numbed with eye drops prior to administration. Side effects can include redness, bleeding, irritation and feeling like there’s something in the eye for a short while.
Have there been any recent breakthroughs with treatment for macular degeneration?
Mr Pasu, along with a team at the King Edward VII’s Hospital, has developed a new macular treatment service that diagnoses and treats patients with wet macular degeneration on the same day, as an outpatient.
Also, new anti-VEGF injections are being developed that can be administered less frequently. One, called brolucizumab (Beovu) has recently been approved for use in the UK and may last as long as three months. It’s also thought to be more effective at drying the fluid that accumulates as a result of wet macular degeneration.
Another promising treatment for wet macular degeneration that’s currently at the research stage is retinal gene therapy. This will involve using the body to make its own anti-VEGF and will be an alternative to regular injections. Gene therapy involves inserting a harmless virus (called an adeno-associated virus, or AAV) carrying the anti-VEGF gene into a person’s DNA.
More information
- If you’re concerned about your eye health, speak to your GP or optician as a first point of call. (If you don’t have a GP, you can make an appointment with one of our private GPs.)
- Expert ophthalmology consultants at the King Edward VII’s Hospital Ophthalmology Department specialise in diagnosing and treating eye diseases such as macular degeneration.
- Mr Pasu’s website contains more in depth information and articles on prevention and treatment for macular degeneration.
- The Macular Society also has lots of help and advice on living with macular degeneration.
Article Sections
Latest Hospital News
Should you wish to speak to our press team, please visit Press Enquiries





