
There are many different types of skin cancer, and overall, skin cancer is one of the most common forms of cancer across the world. Skin cancers fall into one of two groups – non-melanoma skin cancer and melanoma skin cancer.
Here, King Edward VII’s Hospital Consultant Dermatologist, Dr Nilesh Morar discusses the different types of skin cancer and what the signs of skin cancer may be.
The difference between non-melanoma and melanoma skin cancers
Non-melanoma skin cancers usually develop slowly over time, in the top, outermost layers of the skin, called the epidermis.
They are usually seen in the skin that is most exposed to the sun on a regular basis, such as on the face, upper arms, chest and shoulders, back and lower legs. Non-melanoma skin cancer is more common in men than women, and in elderly and middle-aged people than in younger people. It is uncommon for a non-melanoma skin cancer to spread to other parts of the body.
Conversely, melanoma skin cancers are less common than non-melanoma skin cancers. These types of skin cancers develop more quickly than non-melanoma types and can spread to other areas of the body if not treated. Melanoma skin cancers tend to affect the legs, back, face and arms.

Types of non-melanoma skin cancers
The top layers of the skin, called the epidermis, is itself broadly made up of two distinct layers of cells. The lower layer of the epidermis, nearest to the hair follicles, contains basal cells and the upper layer contains squamous cells.
The majority of non-melanoma skin cancers fall into two main categories – basal cell carcinomas (BCC) and squamous cell carcinomas (SCC), depending on where they begin to develop.
Around 75% of all non-melanoma skin cancers are basal cell carcinomas whilst squamous cell carcinomas make up around 20%. The remaining 5% consists of rarer forms of non-melanoma skin cancers, including Merkel cell carcinoma, Kaposi’s sarcoma and sebaceous gland cancer.
Recognising the signs and symptoms of non-melanoma skin cancer
Non-melanoma skin cancers tend to appear gradually as a small, flat, scaly patch of discoloured skin or a form lump that doesn’t go away. They progress slowly over months or even years.
A basal cell carcinoma will appear as either:
- a patch of red, scaly skin, sometimes with dark brown or black areas within the patch
- a small, shiny lump on the skin that is white or pink in colour and either translucent (see-through) or waxy in appearance.

Basal cell carcinoma lesions may:
- develop an outer, crusty layer
- grow larger in size
- begin to bleed
- begin to look like a skin ulcer
A squamous cell carcinoma will appear as a lump on the skin that feels firm to the touch and is pink in appearance. These lumps may:
- develop a crusty top layer of scales
- become spiky in texture
- become tender
- bleed
- begin to look like a skin ulcer

Rarer forms of non-melanoma skin cancer
Merkel cell carcinoma, Kaposi’s sarcoma and sebaceous gland cancer are all rare types of non-melanoma skin cancer. Merkel cell carcinoma is a very rare, but aggressive form of non-melanoma skin cancer. It’s usually only seen in older people and can return in the same place even after successful treatment. This type of skin cancer can also spread to the lymph nodes.
Kaposi’s sarcoma is more common in people with HIV, but those without HIV can also develop this type of non-melanoma skin cancer. It develops within the cells of the lining of the blood vessels that supply the skin with blood.
The sebaceous glands sit within the epidermis and are responsible for producing sebum, the wax-like substance that naturally oils the skin. Sebaceous gland cancer can occur anywhere on the body and is characterised by firm lumps, that don’t feel tender to touch and can often look yellow. This type of cancer is most common in older people and usually appears in the upper eye lid or around the eye. Less commonly, it can also form elsewhere on the head, neck or chest.
Conditions related to non-melanoma skin cancer
There are two other skin conditions, called actinic keratoses and Bowen’s disease that pose a small risk of an individual developing a non-melanoma skin cancer if they’re not treated.
Actinic keratoses is a condition caused by repeated exposure to the sun, year after year. It develops as small (1-2mm to 1-2cm in diameter) scaly patches of dry skin that can vary from pink to red to brown. These patches can thicken and become rough and spiky.
Bowen’s disease develops as a scaly, red patch of skin that can become itchy. It’s most commonly seen on the legs, but these patches can develop elsewhere on the body.
Types of melanoma skin cancers
The most common melanoma skin cancer is a superficial spreading melanoma. This kind of melanoma is a mole that usually grows outwards, across the top of the skin, rather than downwards into the deeper layers of the skin, hence the name superficial.
Superficial spreading melanomas can begin to grow downwards if left untreated, which means that they can spread to different parts of the body.
Other types of melanoma skin cancers include:
- Nodular melanomas – red, dark brown or black raised moles that grow downwards fairly quickly. It’s quite common for these melanomas to bleed.
- Lentigo maligna melanomas – often begin as a flat freckle that gets darker and more apparent than other freckles as it spreads sideways. If left untreated, these melanomas can begin to grow downwards and form a lump.
- Acral lentiginous melanomas – usually found on the palms and soles of the feet, this type of melanoma is very rare and is the most common melanoma in those with darker skin.
- Amelanotic melanoma – often with no colour, or a light pink or red colour, these melanomas are rare and can develop grey or light brown edges.
The NHS has images of all types of melanoma skin cancers listed here to help you if you think you may have a melanoma. If in doubt, always see your GP or specialist.

Recognising the signs and symptoms of melanoma skin cancer
The majority of melanoma skin cancers develop within a mole, which then begins to form an irregular shape and can become multi-coloured. They appear either as a new mole with these features or within an existing one that has begun to change shape and colour. Most melanomas are larger than normal moles and can become itchy and sometimes bleed.
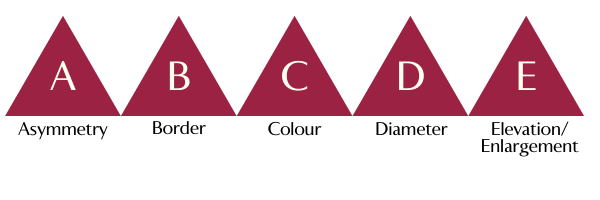
There is a helpful ABCDE of moles checklist that helps identify the difference between a melanoma skin cancer and a normal mole. Potential melanomas may have the following features:
- Asymmetry – an irregular shape, rather than round and even
- Border – blurred edges, rather than distinct, smooth edges
- Colour – a mix of colours including pink, red, brown and black
- Diameter – larger than 6mm (although melanomas can still be smaller)
- Elevation/Enlargement – raised above the surface of the skin
Diagnosing skin cancer
If you’re worried about skin cancer or a mole that’s changing shape, then your GP will be able to advise you on what to do next.
If your GP is concerned, then you will generally be referred to a skin cancer specialist within two weeks. Alternatively, you can see a private skin cancer specialist such as those at the Kind Edward VII Hospital.
Your specialist will usually take a biopsy of the suspected skin cancer, a minor surgical procedure performed under a local anaesthetic. The results of this will tell the specialist if you have skin cancer, and which type.
For basal cell non-melanoma skin cancer, no further tests are generally required before treatment as it’s unlikely that it will spread. For squamous cell non-melanoma skin cancer, your specialist may need to take a biopsy from a lymph node (called a fine needle aspirate, again carried out under a local anaesthetic) to see if it’s spread to the lymph nodes.
In the case of a melanoma skin cancer, your specialist will want to see if it has spread to other parts of the body, beginning with the lymph nodes. You may need to have a procedure called a sentinel lymph node biopsy, performed under a general anaesthetic.
If this test proves positive, then you’ll require further tests to see how far the cancer has spread. These tests include CT, MRI and PET scans. You may also need a procedure called a lymph node dissection or completion lymphadenectomy to remove your lymph nodes.
More information
● If you are concerned about skin cancer, or you have a mole or lump that is changing shape or colour or you have a skin lesion or patch of discolouration that won’t heal, make an appointment to see your GP straight away. (Don’t have a GP?)
● The Kind Edward VII’s Hospital Dermatology Department offers specialised skin cancer treatments including non-surgical treatments and those that minimise skin loss and scarring.
Article Sections
Latest Hospital News
Should you wish to speak to our press team, please visit Press Enquiries





