
Arthritis is a medical condition that affects the joints, causing pain and inflammation. It’s a common condition, impacting more than 10 million people in the UK.
Anyone of any age can suffer with arthritis, including young children. There are many different forms of the condition, including osteoarthritis and rheumatoid arthritis.
Osteoarthritis is the most common form of the condition in the UK, and is caused by wear and tear in the joints. The cartilage that cushions the joints wears away and bones rub against one another, causing the pain associated with osteoarthritis.
Rheumatoid arthritis arises when the immune system incorrectly targets and therefore damages the joints, leading to inflammation and swelling. Both osteoarthritis and rheumatoid arthritis can cause severe pain and discomfort.
There is no cure for arthritis. Instead, those with the condition can only manage their symptoms with lifestyle changes, medications, physiotherapy and sometimes surgical procedures to help slow its onset.
If you have recently had a diagnosis of arthritis, or your doctor suspects that you might have it, then you’ll probably have lots of questions about living with the condition. One such question is around exercise – can you exercise with arthritis and if so, what are the best, and safest, exercises to do?
In this article, King Edward VII’s Hospital sports and exercise physician, Dr David Porter, talks about exercising with arthritis and how to do so safely.
Does exercise help arthritis?
Arthritis can make everyday tasks such as moving, walking and travelling painful and distressing. If you suffer with the pain and discomfort of arthritis, then exercise may be far from your mind.
However, regular exercise can help arthritis sufferers in various ways. Exercise can help to:
- Increase the strength and flexibility of your muscles
- Improve your range of movement
- Improve the mobility of your joints
- Reduce joint stiffness
- Preserve the density of your bones
- Improve your energy levels
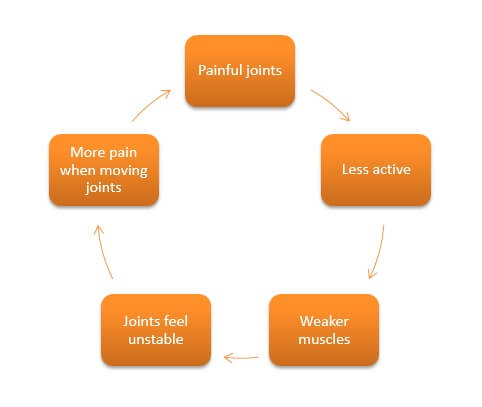
All of these factors can help to reduce the amount of pain you experience and may help to prevent your discomfort from getting worse. It’s easy to become locked in the ‘deconditioning cycle’ if you have arthritis. This cycle starts with painful joints, which leads to being less active. This then means that the muscles become weaker, leading to unstable joints and more joint pain when you do move, completing the cycle.
The deconditioning cycle
Exercise (and eating a healthy, balanced diet) will also help you to manage your weight, in turn minimising any extra load on the joints.
So exercising is important if you’ve been diagnosed with arthritis. But you need to make sure you’re doing the right kinds of exercises that help to support your joints, rather than put unnecessary strain on them.
What is the best exercise for arthritis sufferers?
The charity Versus Arthritis recommends at least 30 minutes of exercise, five times a week, with exercise that makes you a little short of breath. Versus Arthritis also recommend spending at least half an hour each day on your feet, walking or climbing stairs.
Pick exercise that you enjoy. That way, you’re more likely to stay motivated and remain as active as possible. That said, it’s better to choose low impact exercise that puts less pressure on the joints.
Low impact exercises include: walking, swimming, aqua aerobics and cycling, but you can still push yourself whilst doing these exercises if you wish to. Having arthritis doesn’t mean that you can’t carry out low impact exercises vigorously – you just need to be careful to stay within your limits.
Strengthening exercises such as Pilates and yoga are also important to help strengthen your muscles and support your joints. If you’re experiencing a flare up and your joints feel inflamed, hot and swollen, avoid strengthening exercise until your flare up has passed.
Some arthritis sufferers like to use hand weights, but it’s best to stick to very light weights that you can lift easily, with a high number of slow, controlled repetitions. For example, two or three sets of 8-12 reps on each of the following exercises is a good guide:
- Triceps extensions: Use both hands to hold a weight overhead. Keep your elbows pointed upward and lower the weight behind your head. Raise weight overhead and repeat.
- Bicep curls: Begin with arms down at your sides, palms facing outward. Keeping your upper arm at your side, bend at the elbow and bring one dumbbell up to your shoulder. Lower to original position and repeat with opposite arm. Repeat, switching between sides.
- Side lateral raises: With arms down at your sides, palms facing each other, raise slightly bent arms to shoulder height, with palms facing the ground. Lower and repeat. You can do this seated if you wish.
Exercises for rheumatoid arthritis
All of the above exercises can be beneficial regardless of the type of the arthritis you have, although it’s important you don’t push yourself too hard and stop if you feel any pain.
But for rheumatoid arthritis specifically, stretching can be hugely beneficial as it helps to relieve the stiffness of your joints. Try to stretch daily if you can. The type of stretches that can help vary from person to person, but it’s good to focus on gently moving the knees, hands and elbow joints, holding your stretch for 10-20 seconds and repeating it 2-3 times.
You are also highly likely to be prone to hand dysfunction if you have rheumatoid arthritis. Hand exercises can help: try squeezing a stress ball, slowly curling your fingers, spreading them out wide on a table and bending your wrists up and down to improve hand flexibility and strength.
Exercises for osteoarthritis
All forms of low impact exercise are useful for osteoarthritis. Swimming is particularly helpful, however, because the water’s buoyancy reduces pressure on your spine, so your back joints are less likely to get irritated and the risk of possible injury is lower. Swimming also counts as resistance exercise, so your muscles get stronger.
In terms of stretching, your focus should really depend on where your osteoarthritis is located – is it spinal, in your knee or hip? Neck and back exercises help to protect the spine. Add resistance by using exercise bands – this can make a real difference. If you have osteoarthritis that’s situated in the knee or hip, stretching out your quadriceps, calves, doing leg raises and step-ups can all help to ease your joints. This video outlines how to do some of these exercises.
Make sure you exercise safely
It’s normal to feel sore and stiff after exercise, especially if you’re new to a particular exercise, or exercise as a whole. This doesn’t necessarily mean that you’ve damaged your joints further, and can often mean the opposite. Soreness should usually disappear after a couple of days.
As much as exercise is important to help to manage your condition, you need to exercise carefully and safely – avoid putting too much pressure on your joints or overexerting yourself. If you ever feel pain from exercising that’s unbearable or it feels like it could be doing you damage, then stop. Listen to your body and rest when you feel you need it.
Speak with your care team about the best exercises to suit your personal circumstances. They will provide you with advice and lifestyle tips on how best to keep your arthritis pain and discomfort under control.
More information
- Your GP is a good first port of call if you think you may be suffering with the symptoms of arthritis. They can refer you to a specialist for tests, who can then discuss your treatment options with you. (Don’t have a GP?)
- Dr David Porter is an expert in performance-focused sports and exercise medicine and can provide advice and guidance on exercising safely with arthritis. Make an enquiry.
Article Sections
Latest Hospital News
Should you wish to speak to our press team, please visit Press Enquiries





